Rabies is an infectious viral disease that is almost always fatal following the onset of clinical symptoms. In up to 99% of cases, domestic dogs are responsible for rabies virus transmission to humans. Yet, rabies can affect both domestic and wild animals. It is spread to people through bites or scratches, usually via saliva.
World Rabies Day is the first and only global day of action and awareness for rabies prevention. It is an opportunity to unite as a community and for individuals, NGOs and governments to connect and share their work.
September 28th, 2019 is the 13th World Rabies Day, and this year’s theme focuses on vaccination, the foundation of all rabies control efforts.
The theme, Rabies: Vaccinate to Eliminate, can be used to raise awareness at many levels:
• To ensure that dogs are kept vaccinated – as a reminder to dog owners, animal health professionals and local governments
• To help people in need to seek and obtain PEP (Post Exposure Prophylaxis) – through human health professionals and educators. PEP is the immediate treatment of a bite victim after rabies exposure.
• To commit to the 2030 goal of eliminating rabies deaths – with national governments putting resources into rabies elimination
Rabies is present on all continents, except Antarctica, with over 95% of human deaths occurring in the Asia and Africa regions.
Rabies is one of the neglected tropical diseases that predominantly affect poor and vulnerable populations who live in remote rural locations. Although effective human vaccines and immunoglobulins exist for rabies, they are not readily available or accessible to those in need. Globally, rabies deaths are rarely reported and children between the ages of 5–14 years are frequent victims.
According to WHO, more than 15 million people worldwide receive a post-bite vaccination every year. This is estimated to prevent hundreds of thousands of rabies deaths annually.
Prevention

Eliminating rabies in dogs
Rabies is a vaccine-preventable disease. Vaccinating dogs is the most cost-effective strategy for preventing rabies in people. Dog vaccination reduces deaths attributable to rabies and the need for PEP-post exposure prophylactics – as a part of dog bite patient care.

Awareness on rabies and preventing dog bites
Increasing awareness of rabies prevention and control in communities includes education and information on responsible pet ownership, how to prevent dog bites, and immediate care measures after a bite.
Preventive immunization in people
Human rabies vaccines exist for pre-exposure immunization. These are recommended for people in certain high-risk occupations such as laboratory workers handling live rabies and rabies-related (lyssavirus) viruses; and people (such as animal disease control staff and wildlife rangers) whose professional or personal activities might bring them into direct contact with bats, carnivores, or other mammals that may be infected. Also, immunization should be considered for children living in high risk area, as they play with animals.
Symptoms
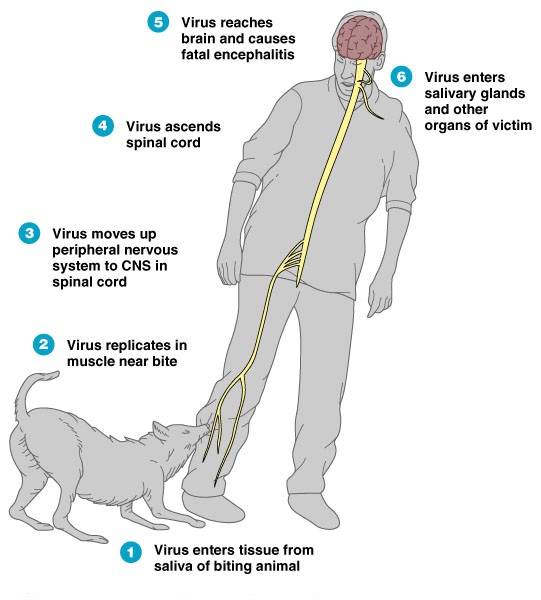
The incubation period for rabies is typically 2–3 months but may vary from 1 week to 1 year, dependent upon factors such as the location of virus entry and viral load. Initial symptoms of rabies include a fever with pain and unusual or unexplained tingling, pricking, or burning sensation (paraesthesia) at the wound site. As the virus spreads to the central nervous system, progressive and fatal inflammation of the brain and spinal cord develops.
There are two forms of the disease:
• People with furious rabies exhibit signs of hyperactivity, excitable behaviour, hydrophobia (fear of water) and sometimes aerophobia (fear of drafts or of fresh air). Death occurs after a few days due to cardio-respiratory arrest.
• Paralytic rabies accounts for about 20% of the total number of human cases. This form of rabies runs a less dramatic and usually longer course than the furious form. Muscles gradually become paralyzed, starting at the site of the bite or scratch. A coma slowly develops, and eventually death occurs. The paralytic form of rabies is often misdiagnosed, contributing to the under-reporting of the disease.
Diagnosis

Current diagnostic tools are not suitable for detecting rabies infection before the onset of clinical disease, and unless the rabies-specific signs of hydrophobia or aerophobia are present, clinical diagnosis may be difficult.
Transmission
People are usually infected following a deep bite or scratch from an animal with rabies, and transmission to humans by rabid dogs accounts for 99% of cases. Africa and Asia have the highest rabies burden in humans and account for 95% of rabies deaths, worldwide.
In America, bats are now the major source of human rabies deaths as dog-mediated transmission has mostly been broken in this region. Bat rabies is also an emerging public health threat in Australia and Western Europe.
Transmission can also occur when infectious material – usually saliva – comes into direct contact with human mucosa or fresh skin wounds. Human-to-human transmission through bites is theoretically possible but has never been confirmed.
Contraction of rabies through inhalation of virus-containing aerosols or through transplantation of infected organs is rare. Contracting rabies through consumption of raw meat or animal-derived tissue has never been confirmed in humans.
Post-exposure prophylaxis (PEP)
Post-exposure prophylaxis (PEP) is the immediate treatment of a bite victim after rabies exposure. This prevents virus entry into the central nervous system, which results in imminent death. PEP consists of:
• Extensive washing and local treatment of the wound as soon as possible after exposure. It includes immediate and thorough flushing and washing of the wound for a minimum of 15 minutes with soap and water, detergent, povidone iodine or other substances that kill the rabies virus
• A course of potent and effective rabies vaccine that meets WHO standards; and
• The administration of rabies immunoglobulin (RIG), if indicated.