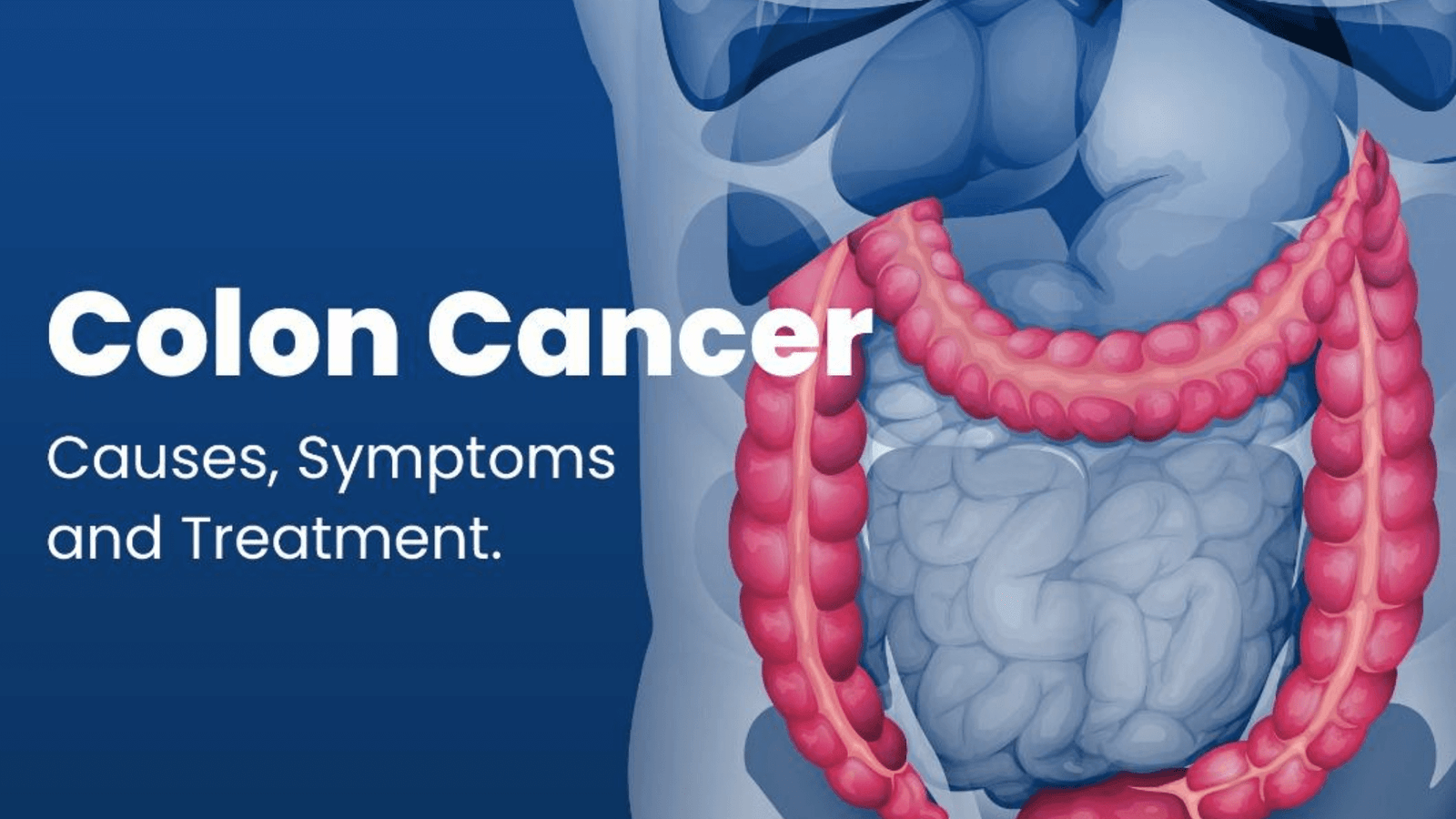
The Colon is the large intestine or large bowel. The rectum is the passageway that connects the colon to the anus. Sometimes abnormal growths, called polyps, form in the colon or rectum. Over time, some polyps may turn into cancer. Screening tests can find polyps so they can be removed before they turn into cancer.
Colon cancer is sometimes called Colorectal cancer, which is a term that combines colon cancer and rectal cancer, which begins in the rectum. It is the third most common cancer worldwide and the second type that accounts for more cancer deaths.
Causes of colon cancer
Together, the colon and rectum make up the large intestine. The colon, which is about four feet long, helps digest food and remove nutrients and water before sending the waste to the rectum, the final few inches of the intestine. Cancer may develop when:
- Polyps, mushroom-like growths inside the colon, grow and become cancerous
- Cells along the lining of the colon or rectum mutate and grow out of control, forming a tumor
Risk factors for colon cancer include:
- Genetics:
- Family history: the reasons are not clear in all cases, inherited genes, shared environmental factors or a combination of these influences may increase your risks. Your family history may determine when your doctor will recommend a colonoscopy to screen for colon or colorectal cancer. For example, if your father was diagnosed at 50, your doctor may recommend you get a colonoscopy at 40.
- Racial and Ethnic background: African American men and women are at a significantly higher risk of developing colon cancer. People of Ashkenazi Jewish descent have a higher risk too.
- Lifestyle:
- Tobacco use
- Sedentary lifestyle
- Heavy alcohol use
- Poor diet, especially high in red and processed meats
- General
- Age: Although colon cancer may occur at any age, the chances of developing the disease may dramatically increase after the age of 45. Nearly 95 percent of all cases occur in patients 45 or older.
- History of previous colon cancer or polyps: If you have had colon cancer before, you are more likely to develop cancer in other areas of the colon and rectum. On the other hand, you may experience a recurrent cancer, which is a malignancy that reappears at or near the same location as the original tumor. You may also be at a higher risk if your doctor found polyps during a colonoscopy, even if those polyps were removed and/or benign.
- History of inflammatory bowel disease (IBD): Having IBD, including ulcerative colitis and Crohn’s disease, may increase your chances of developing colon cancer. Your risk may be higher the longer you have experienced IBD and depending on how much of your colon is affected.
- Obesity: Being overweight may increase your risk of developing colorectal cancer.
- Type II diabetes: This condition is associated with a higher risk of rectal cancer. It may also affect your prognosis.
Symptoms
- Diarrhea, constipation or both
- Thin, ribbon-like stools
- Abdominal bloating or cramps
- Feeling as if the bowel does not empty completely
- Rectal bleeding or blood in the stool
- Loose or watery stools
- Unexplained weight loss and/or loss of appetite
Diagnostics and Screening
Colorectal cancer may be detected and treated early with a proper screening regimen. Men and Women of average or low risk have a colonoscopy beginning at age 45. African Americans have a higher risk of colorectal cancer and should begin screening at the age of 45.
People with a family history of colorectal cancer should be screened 10 years earlier than when a family member was diagnosed. For example, talk to a doctor about getting a colonoscopy at 35 if your father was diagnosed with colon cancer at 45.
During a colonoscopy, a doctor may be able spot cancer in its early stages, perform a biopsy and remove polyps that may develop into cancer. For some patients who choose not to get a colonoscopy, less invasive stool tests [occult blood tests or Fecal Immunochemical(FIT) tests] may be an option.
Treatment
Surgery is most often the first-line treatment for colorectal cancer.
Other treatments include:
Chemotherapy, Radiation therapy, Targeted therapy, Immunotherapy